Personalised care through pharmacogenetics
In late 2019, fifty general practitioners from Zorggroep Zorroo, Zorggroep Het Huisartsenteam and Medisch Centrum de Poort, together with Star-shl and the Netherlands Pharmacogenetics Expertise Centre, started the pharmacogenetic diagnostics pilot. The pilot started off with a fantastic training course by Prof. R. van Schaik.
Individuals may respond differently to medicines. Some of these differences are due to the personal genetic profile – variations in DNA. These decide, among other things, how quickly the drug is metabolised by liver enzymes. Using pharmacogenetic research, an explanation can be found as to why a specific drug is ineffective or produces side effects in an individual. The question is how this personalised medicine can contribute to the quality of life of a patient being treated with antidepressants.
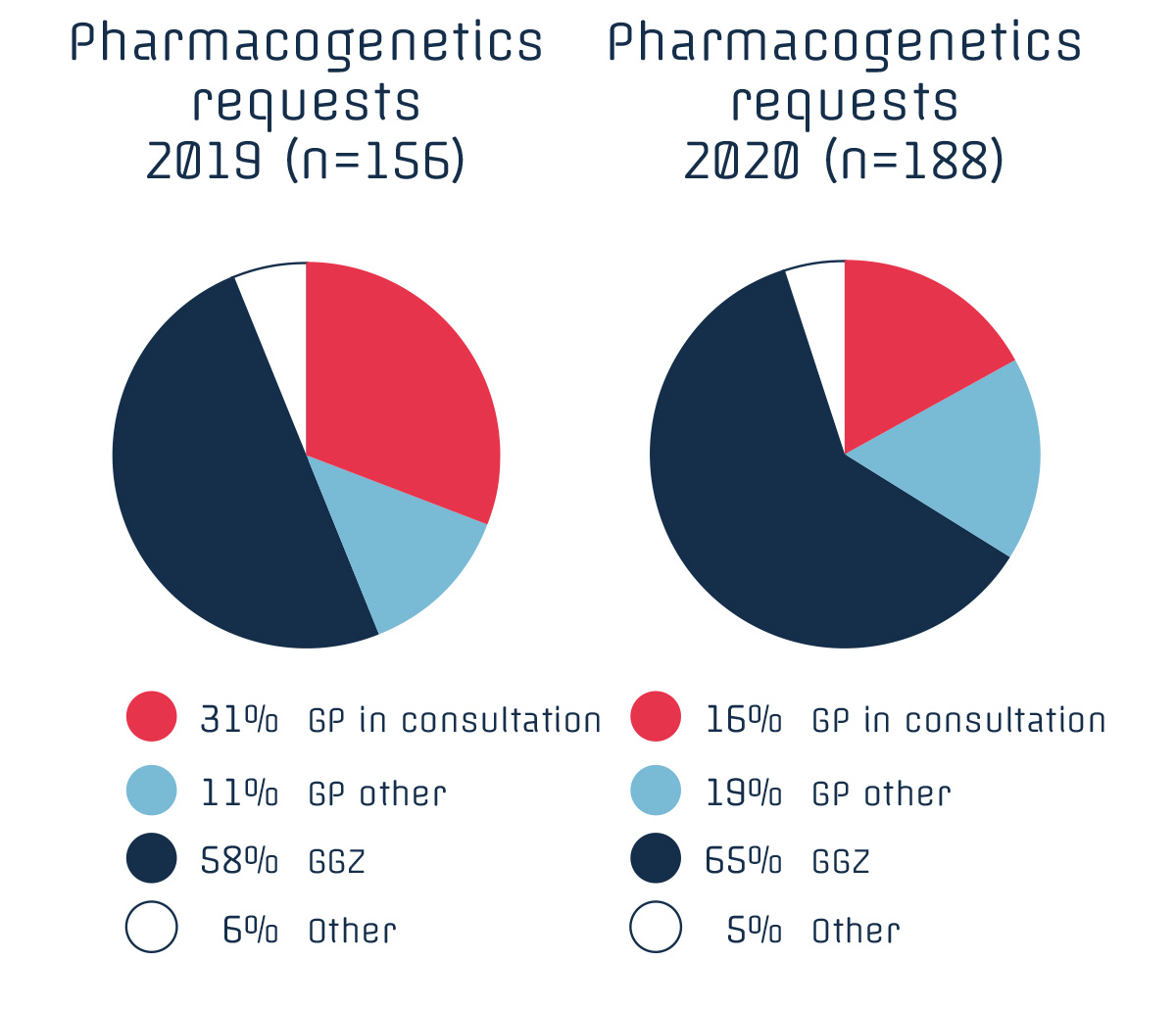
In many publications, we read that psychological problems are increasing the pressure on GP practices and that this is being intensified by COVID-19. This could lead to increased requests for pharmacogenetic research, given its added value in the prescription of psychopharmaceuticals. However, requests for pharmacogenetics from general practitioners actually decreased with the increase in the number of patients with COVID-19.
The general practitioners had other priorities than gaining experience with new diagnostics. After the summer, more applications came in and new general practitioners registered. In response to this, the project group decided to extend the project until early 2021.
The total number of applications in 2020 has increased, despite COVID-19, mainly due to an increase in applications from the GGZ and general practitioners outside the project. It is noteworthy that an increasing number of general practitioners make incidental use of various indications for pharmacogenetic diagnostics.
For the time being, the DNA passport for the patient remains a physical card that is highly valued by the patient. All project documents, such as application forms and patient leaflets, are available digitally and up to date at https://www.star-shl.nl/zorgverlener/farmacogenetica/.
The current version of the table with relevant enzymes and substrates can also be consulted on this website, as well as background information such as NHG’s viewpoint on pharmacogenetics.
In early 2021, the project will be evaluated and we will know whether pharmacogenetics help GPs to provide more effective therapy with fewer side effects.
The Jan Schueler Foundation is supporting this initiative on the basis of its objective to make new laboratory diagnostics available for primary care.
